Autonomous Dysreflexia And Its Dangers
Autonomous dysreflexia is a disorder that can lead to death if not properly treated. Bone marrow injuries are one of the most common causes of their occurrence.
The Autonomous dysreflexia is a disorder that can lead to death if not treated appropriately. Bone marrow injuries are among the most common causes of their occurrence.
With this complication, patients have spinal cord injuries in a chronic phase. It occurs in 85% of people who have had severe damage to the seventh thoracic spine, the T7.
It is an abnormal and excessive nervous system response that is uncontrolled or autonomous to stimulation. The Autonomous dysreflexia can cause changes in heart rate, profuse sweating and high blood pressure, among other symptoms.
Autonomic dysreflexia and its causes

One of the most common causes of autonomic dysreflexia is spinal cord injury. A patient suffering from this will show strong responses to various stimuli that would not affect a healthy person.
However, it can also be triggered by other reasons, such as Guillain-Barré syndrome. This is a disorder in which the immune system mistakenly attacks parts of the nervous system.
Side effects of some medications as well as severe skull and brain injuries such as subarachnoid hemorrhage can also lead to this condition. The use of illegal stimulants such as cocaine and amphetamines are other causes of autonomic dysreflexia.
Symptoms
In the area under the injured spinal cord, the skin is pale and uncontrolled muscle contractions ensue. In contrast, redness is visible in the areas above the injury, there is profuse sweating and pupillary dilation or mydriasis.
The patient may also experience headache, chest pain, anxiety, shortness of breath, or blurred vision. Furthermore, impaired consciousness, convulsions and cerebral haemorrhage can occur. In these cases, autonomic dysreflexia should be treated as an emergency.
Other possible symptoms are:
- Intestinal discomfort
- fever
- Nasal congestion
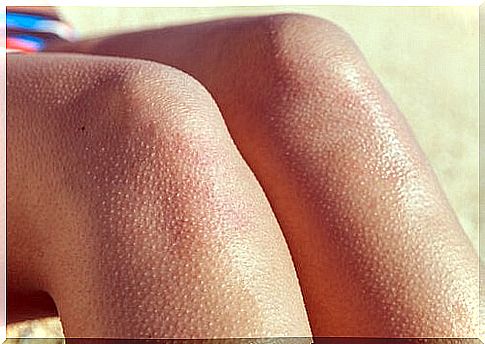
- goose bumps
Despite the symptoms mentioned, it is possible that autonomic dysreflexia will not make itself felt – even if the blood pressure rises dangerously.
Preventing autonomic dysreflexia
To prevent autonomic dysreflexia, drugs that could cause it due to their side effects should be avoided.
People who have already had a bone marrow injury should follow medical advice to avoid this complication. First and foremost, it is important to prevent an over-filled bladder, which is why it is important to urinate frequently.
Suppressing bowel movements should also be avoided. In addition, care must be taken to keep the feeling of pain under control. This also includes taking care of the skin so that ulcers and infections do not develop.
Prognosis and possible complications
The prognosis depends primarily on the cause of the disorder. If the autonomic dysreflexia is the result of drug treatment, patients usually recover when it is appropriately prevented.
However, if other factors were causing the problem, recovery will depend on how treatable the disorder is.
Potential complications may arise in connection with the side effects of the medication being administered. Severe and long-lasting high blood pressure can lead to the following complications:
- cramps
- Bleeding in the eyes
- stroke
- death
treatment

Autonomic dysreflexia can lead to death. It is therefore important to be able to identify them immediately and to have them treated. Treatment takes place in connection with the cause of the disorder. If it was caused by certain medications , these must be discontinued.
If the heart rate is the triggering symptom, anticholinergics such as atropine may be given. But it is also important to treat high blood pressure as quickly as possible. However, this should be done with care so that it does not suddenly drop.
Finally , if the heartbeat is irregular, the patient should wear a pacemaker.